Clinical studies begin on a tiny technology that could pinpoint arterial disease risks
By Julia Evangelou Strait
Learn More
A new nanoparticle-based imaging agent may help identify patients at high risk of stroke by revealing dangerous plaque in arteries. The Food and Drug Administration (FDA) has approved the agent for investigational use in people. The technology was jointly developed at Washington University School of Medicine and the University of California, Santa Barbara, in collaboration with Texas A&M University.
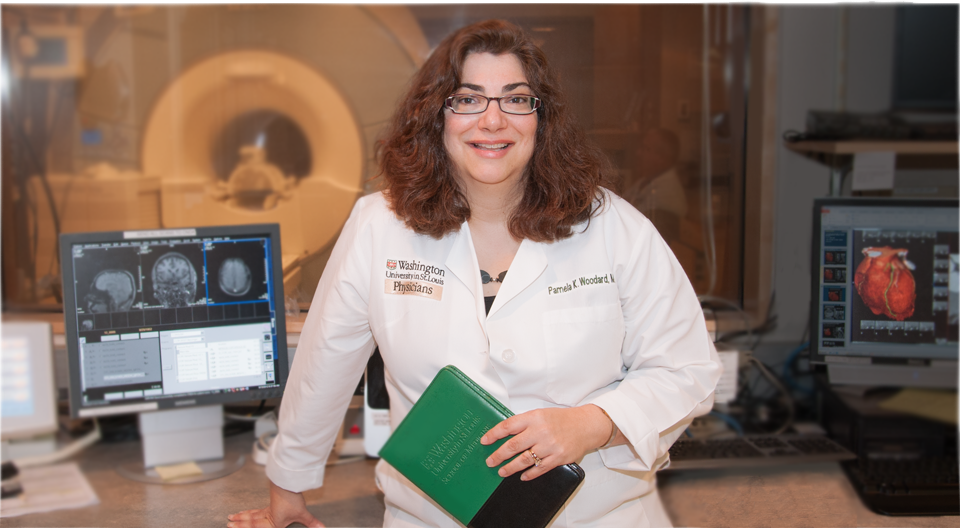
“This is the first receptor-targeted nanoparticle agent for cardiovascular imaging approved for investigational use in humans,” said principal investigator Pamela K. Woodard, MD, professor of radiology and of biomedical engineering. “Starting with bench research, then developing and testing the agent and taking it through the FDA process into human patients has involved an extensive team of basic scientists, clinical researchers and clinicians.”
Pinpointing plaque
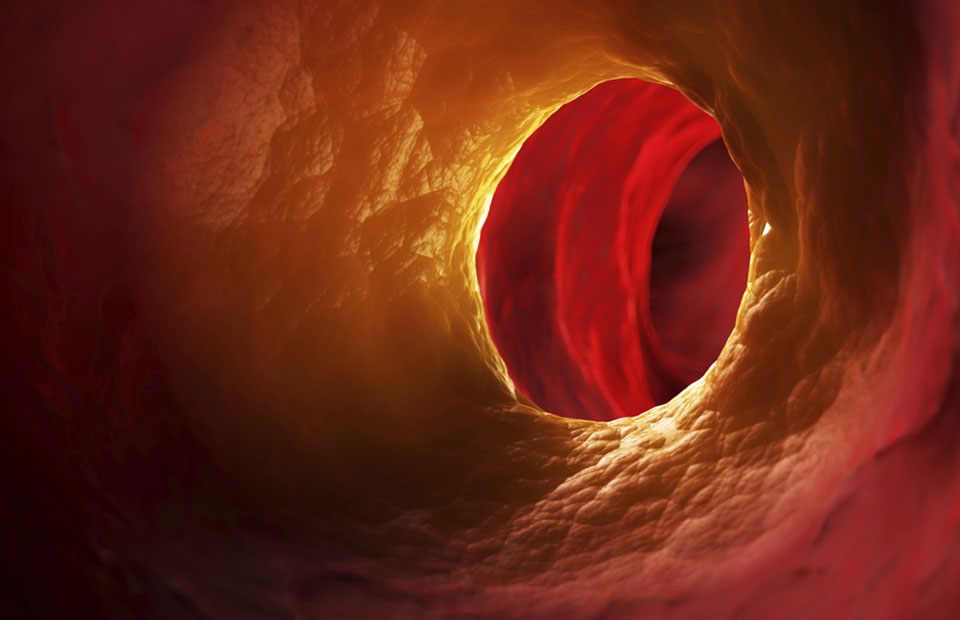
In patients with atherosclerosis, plaque accumulates on the inner walls of arteries, which deliver blood to the body. In many cases, the accumulated plaque causes no symptoms and remains undiagnosed by physicians. Plaque accumulation eventually can narrow an artery enough to cause chest pain or mild symptoms. But, for some, this plaque suddenly can rupture without warning, create blockages and cause a heart attack or stroke.
“Plaque is a complex structure, made up of cholesterol, calcified deposits and other substances, all of which can cause plaque instability,” said Woodard, also director of the Center for Clinical Imaging Research (CCIR) at the Mallinckrodt Institute of Radiology at Washington University.
“This imaging agent targets a specific receptor that is present in more vulnerable complex plaque, thereby identifying which plaques might rupture in the patient, leading to stroke or heart attack.”
Past research shows most patients with plaque narrowing a carotid artery will not go on to have a stroke.
Distinguishing high-risk patients
“With current technology, such as ultrasound, we can’t tell whether the plaque is vulnerable or stable,” she said. “So we can’t distinguish the high-risk patients who need surgery from low-risk patients who can be treated with medication alone.
“We designed this nanoparticle agent to develop a test that can detect these vulnerable plaques and identify those patients at highest risk of stroke and in need of surgery to remove the plaque.”
Gregorio A. Sicard, MD, vascular surgeon and professor of surgery and of radiology, said specialists who treat carotid artery disease have been seeking a diagnostic test that could identify extracranial carotid artery disease, which is more prone to embolize, rupture or occlude the carotid artery. These types of vulnerable plaques are more likely to cause an embolic cerebral vascular event with devastating effects. In many cases, these patients are asymptomatic.
“This exciting work by Dr. Woodard and collaborators may provide a screening imaging study that will identify, in asymptomatic patients, those that have a vulnerable plaque and are therefore more likely to have a cerebral vascular event,” Sicard said. “This cutting-edge diagnostic study hopefully will revolutionize the management of patients with asymptomatic carotid plaque and plaque in other arterial beds.”
Miniaturized medicine
The nanoparticle-based imaging agent carries custom peptide molecules that bind to the receptors of unstable plaques. First, the peptides are attached to nanoparticle “combs,” left, which morph into star-like shapes when wetted. Injected into the bloodstream, legions of these stars descend on dangerous plaques, shining brightly on radiologic images.
How it works
The nanoparticle is unique in how it is targeted, according to Yongjian Liu, PhD, assistant professor of radiology and co-investigator on the project. Previous research demonstrated that a receptor called NPR-C is present on the surface of cells that line blood vessels and is increased in plaque associated with atherosclerosis. So the investigators added a small peptide to the nanoparticle. That peptide seeks out and binds to NPR-C, specifically targeting the particle to potentially dangerous plaque.
The nanoparticle also carries copper atoms, making it visible with a standard positron emission tomography (PET) scanner. Similarly, small amounts of copper-64 are used in PET scans for cancer detection and therapy and neurologic imaging. Once injected, this nanoparticle agent can illuminate potentially vulnerable plaque in the body’s arteries.
The carrier nanoparticle was crafted in the lab of Craig J. Hawker, PhD, professor and director of the California Nanosystems Institute at the University of California, Santa Barbara.
“We couldn’t carry out the research without his contributions,” Woodard said.
Following successful tests in animal models, researchers recently began testing the safety of the nanoparticle in healthy individuals. Next, they will focus on patients with atherosclerosis who already are scheduled to undergo surgery to remove plaque from their carotid arteries.
Testing of these patients will begin in a novel PET-MR system housed in the CCIR, so that the researchers can look at plaque anatomy on MRI and PET signals from the new agent concurrently.
“We’ll be able to see whether the areas that light up in the image because of our nanoparticles are the same areas that contain vulnerable plaque, as assessed from the surgeries,” Woodard said.
Once the investigators demonstrate success imaging the carotid arteries, they will evaluate the nanoparticle agent in other vessels such as the coronary arteries, which represent a greater challenge because of their smaller size and complex motion.
“Given the clinical success of this agent, with the assistance of the Office of Technology Management, we have begun seeking to advance this imaging agent into a commercial product,” Woodard said.
“We have been able to develop this highly receptor-specific imaging technology because of the generous support from the National Heart, Lung and Blood Institute, our diverse and dedicated team of investigators and our extensive facilities at Washington University,” she added.






