


Search and Destroy:
The Immune System vs. Tumors
Colds and cancer are different, right? But shouldn't the body's defensive gatekeeper—the immune system—guard against both? Research stood in the face of common sense—until now.
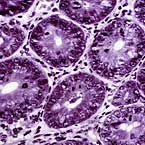
The enemy within: tissue sample of a tumor.

Combined with mounting evidence in the field, it's a discovery that could redirect the pursuit of cancer therapies and our understanding of how the human body responds to infection.

GLOSSARY
Lymphocytes White blood cells (immune cells) that detect and kill foreign or diseased cells
RAG2 Gene found in all lymphocytes
IFN gamma Protein produced by lymphocytes that helps the immune system
Stat1 Protein required for IFN gamma to function
TAP1 Protein found in low levels in many tumors that escape immune system detection
Doubly-deficient Mice lacking RAG2 and Stat1
![]()
Chicken soup may soothe the throat or calm an aching tummy, but the immune system ultimately is the body's real hero, scouring it for danger and defending it against suspect cells. But what about tumor cells? Does the immune system also protect against these often deadly enemies?
For years scientists expected it did. But studies in the 1970s found that “nude” mice—those thought to lack immune cells called lymphocytes—did not develop more chemically induced or spontaneous tumors than normal mice. The immune system theory was largely abandoned.
But some researchers continued to search for a role of the immune system in tumor development, determined to bridge the gap beween immunology and oncology.
To that end, Robert D. Schreiber, PhD, the Alumni Professor of Pathology and Immunology and professor of molecular microbiology, formed a collaboration with Lloyd J. Old, MD, director and CEO of the Ludwig Institute for Cancer Research at Memorial Sloan-Kettering Cancer Center in New York. Schreiber is known for his research on interferon-gamma (IFN gamma), an important protein in the immune system, while Old is considered by many to be the grandfather of tumor immunology. With help from a team of School of Medicine researchers, the pair have determined that the immune system does in fact appear to protect against tumor formation.
Combined with mounting evidence in the field, it's a discovery that could redirect the pursuit of cancer therapies and our understanding of how the human body responds to infection.

Robert D. Schreiber, PhD, has spent the past eight years exploring whether the immune system is involved in tumor formation. He led the study; Vijay Shankaran, MD, PhD, was first author.
The first flaw in the evidence against the immune system theory was revealed in the mid-1980s, when two separate studies found that nude mice were not in fact completely free of lymphocytes, as previously thought.
Schreiber and others later found signs that both lymphocytes and IFN gamma might play important roles in tumor prevention.
Now, in a paper published in the April 26, 2001 issue of the journal Nature, Schreiber's team presents the first conclusive evidence that lymphocytes and IFN gamma work together to find and eliminate tumor cells.
When a role for the immune system in tumor formation was proposed decades ago, scientists envisioned a process called immunosurveillance. Like a burglar alarm that detects intruders, the immune system was thought to patrol the body, catching cells at the beginning of their transformation into suspicious tumor cells.
In contrast, Schreiber and his colleagues propose a new model called immunoediting. Like the security guard, editors catch errors and delete them. They also adjust and tweak areas that need smaller alterations. According to immunoediting, the immune system constantly eliminates certain types of tumor cells and also changes the characteristics of others.
“This sheds light on an age-old controversy and suggests
new possibilities for cancer therapy,” says Schreiber. ![]()
|
FOUR KEY FINDINGS: The immune system eliminates some tumor cells, changes the characteristics of others. 1. Lymphocytes and IFN gamma help prevent formation of chemically induced tumors Schreiber's team first examined whether mice lacking lymphocytes developed tumors when exposed to a chemical carcinogen. To do so, they developed a strain of mice that definitively lacked functional lymphocytes. This was accomplished by inactivating a gene found in all lymphocytes, RAG2. They then injected the chemical carcinogen MCA into a group of mice lacking RAG2 and into a group of normal mice. Only 19 percent of normal mice developed tumors, in contrast with 58 percent of RAG2-deficient mice. In previous studies, the group examined the effect of MCA on mice lacking either the receptor for IFN gamma or one of the proteins required for the receptor to function, Stat1. Roughly half of these mice also developed tumors. In their current study, the researchers also generated mice with two disrupted genes—the gene for RAG2 and the gene for Stat1. When these doubly-deficient mice were injected with MCA, 72 percent of them developed tumors. Statistically, this was not greater than the incidence of tumors in mice that lacked just one gene or the other. Therefore, the team concluded that RAG2 and the IFN gamma receptor have overlapping roles. “We think the two are potentially part of the same mechanism but represent different steps in the process,” explains Schreiber. “IFN gamma makes tumor cells expose themselves to the immune system. After seeing the abnormal proteins in the tumor, the lymphocytes eliminate the tumor cells.” 2. Lymphocytes and IFN gamma help prevent formation of spontaneous tumors Only some human tumors can be directly blamed on chemical carcinogens. Often, tumors develop spontaneously, without any apparent trigger. So Schreiber and colleagues examined whether lymphocytes and Stat1 contribute to the natural development of tumors in the absence of a carcinogen. Again, they studied three groups of mice—normal, RAG2-deficient, and those deficient in both RAG2 and Stat1. After 15 months, two of 11 normal mice had noncancerous tumors and the rest were tumor-free. On the other hand, all 12 RAG2-deficient mice had developed tumors, half of which were cancerous. Particularly surprising was the fact that mice lacking both RAG2 and Stat1 seemed to get very sick very quickly. All 11 doubly-deficient mice developed tumors well before 15 months. Moreover, six developed cancerous tumors in the mammary glands. This type of cancer rarely occurs in RAG2-deficient mice or in young mice lacking the IFN gamma receptor. At first glance, the higher threat of developing spontaneous tumors in doubly-deficient mice seems to contradict the first finding that mice lacking both genes are not at a significantly greater risk of developing chemically induced tumors. But IFN gamma also plays a part in non-immune responses. According to Schreiber, “while the roles of lymphocytes and IFN gamma overlap, IFN gamma also might prevent tumor formation via mechanisms not involving the immune system.” 3. Even a healthy immune system only catches some tumors——those that escape detection pose a greater threat The first two findings show that both IFN gamma and lymphocytes interact with one another to protect individuals from cancer development. That's the good news. But there's also bad news. Tumors that developed in normal mice due to injection of MCA were later transplanted into healthy mice. The tumors continued to grow. Tumors from RAG2-deficient mice also were transplanted into healthy mice. Eight out of 20 of these were rejected. Apparently, the immune systems in healthy, carcinogen-free mice were better equipped to recognize—and reject—tumor cells that developed in RAG2-deficient mice (in the absence of a healthy immune system) than tumor cells that had developed in mice with intact lymphocytes. “As a result of protecting the body, the immune system paradoxically favors the outgrowth of tumors that are less likely to be recognized and killed by the immune system,” Schreiber says. “It's a Ôsurvival of the fittest' scenario that works against the host.” His immunoediting theory may explain this selective protection. “If immunoediting is always occurring, it can have multiple outcomes,” he explains. “If you're lucky, the outcome is protection. But if you're unlucky, transformed tumor cells might alter themselves so the immune system can pick out only a few. The others continue growing.” 4. TAP1 can flag tumors, making them more “visible” to the immune system Some tumors that escape immune detection appear to have low levels of a protein called TAP1. So the scientists added this protein to tumors before transplanting them into healthy mice. This, they hoped, would trick the immune system and allow for easier identification of dangerous cells. When highly aggressive tumors such as those that managed to develop in mice with a healthy immune system were transplanted into healthy mice, they grew in an extremely rapid manner. However, when these tumors first were tagged with TAP1 before being transplanted, they were rejected. When tagged tumors were transplanted into RAG2-deficient mice, they still went unnoticed. Thus, TAP1 facilitated tumor detection and elimination only in the presence of a healthy immune system. “We showed that if a tumor is forced to reveal itself to the immune system, it often is rejected,” Schreiber explains. “We think that a tagged tumor could be used to train the immune system to reject others like it. This is very exciting because it indicates that immunotherapy has a significant potential use even for the treatment of tumors that are altered by the immunoediting process.” |