
In late 2021, Washington University medical student Joshua Perez-Cruet (WUSM 2025) found himself in Senior Associate Dean of Medical Education Eva Aagaard’s office to address an omission in the school’s curriculum. Throughout the entirety of the Gateway Curriculum’s preclinical phase, the health effects of climate change were mentioned only once, tucked into a single paragraph in a required reading.
The disconnect stuck with Perez-Cruet. An avid outdoorsman, he had studied ecology and evolutionary biology, with a resume ranging from managing endangered species in Colorado to studying river-bottom invertebrates as indicators of ecosystem health.
“That single paragraph was about what I expected,” Perez-Cruet said. “The medical school curriculum is already so saturated with content that integrating anything new requires a lot of intentionality and advocacy. What was truly astonishing to me was the scarcity of existing climate curricula for medical schools.”
As the two discussed what could be done, Aagaard suggested Perez-Cruet consider designing sessions for the Gateway Curriculum, as part of the EXPLORE phase Education Pathway.
With the help of faculty mentors and other students, Perez-Cruet has designed sessions for the curriculum’s preclinical phase, each tailored to integrate with various learning modules. In doing so, Perez-Cruet has become a thread leader, a role usually reserved for faculty who manage longitudinal content across modules.
“From my perspective, what Josh and his fellow students have done has been so impressive on so many levels,” said Aagaard, MD, also the Carol B. and Jerome T. Loeb Professor of Medical Education. “With his thoughtfulness and creativity and understanding of the complexity of trying to change a curriculum, he has essentially been approaching the sessions at the level of a thread leader and has made something really valuable from an educational perspective.”

In an educational landscape where doctors traditionally receive little training in environmental health, Perez-Cruet’s sessions stand out. Climate change has become a major driver in public health issues, putting physicians increasingly in the position of explaining its effects. Integrating such content into medical school curricula, however, has been highly variable and often lagging behind what is known about these associations.
“Doctors are at the center of so many decisions in health care and have such a platform,” Perez-Cruet said. “Talking from a health perspective has a really strong potential to resonate with people who wouldn’t otherwise engage in discussions around climate change, such as improving waste sorting in the operating room or choosing sustainable suppliers.”
Becoming more climate-conscious
As it happened, Perez-Cruet’s interest in medical education came right as MedEdPORTAL, a prominent medical education journal, issued a call for papers about teaching students the links between health and climate change.
Perez-Cruet teamed up with Janice L. Hanson, PhD, professor of medicine and the director of education scholarship development and co-director of the Medical Education Research Unit, to hone his research methods and understand the impact of his educational interventions.
“Climate change was a hot topic at the Association of American Medical Colleges (AAMC) meeting last November,” Hanson said. “It was a key theme with a plenary speaker and many sessions devoted to this topic. So that says two things. Medical educators have realized that we need to address climate change and that the AAMC was interested in providing some motivation and information to help schools.”
As part of the trial rollout at WUSM, students chose between four breakout sessions that touched on different aspects of climate change. Through an interactive game, the students then taught each other content from the sessions. Post-session surveys showed that the information increased students’ understanding of the cause and effects of climate change, health care’s contributions to climate change, and opportunities to mitigate these impacts. After the session, nearly every student felt more likely to make future efforts to reduce the environmental impacts of health care.
The content has been integrated into the Gateway Curriculum’s first module, called “Molecules to Society,” for future medical school classes.
“The key with implementing new sessions is to have forward-thinking individuals to constantly revise and think about how the curriculum can get better,” said James Li, MD, an assistant professor of emergency medicine who led one of the breakout sessions. “Climate change can be a political topic, but reframing it by centering on the patient is an important way to look at it. Josh did a great job doing just that.”
Perez-Cruet now is focused on the next curriculum challenge: keeping the environmental health focus going after he graduates. His efforts have expanded to an additional three modules in the preclinical immunology, pulmonology and gastrointestinal units, with four more in the works. In the curriculum’s second module, focused on infectious disease and immunology, Perez-Cruet’s team developed an interactive session that explores the spread of vector-borne diseases as a result of climate change. It concludes with a cancer care case study on the shortage of IV bags after Hurricane Maria shut down Puerto Rican manufacturing plants in 2017. A session on air pollution and wildfires, which dovetails with the pulmonology unit, will equip students with strategies for protecting patients disproportionately impacted by exposures to different air pollutants.
“With the Gateway Curriculum, we’ve been really, really thoughtful about what the right level is that we’re trying to hit for content,” Aagaard said. “It requires an iterative thought process and a partnership with the students to make sure we’re hitting things at the right stage and the right depth. Being thoughtful about this lets us add new content and eliminate content more easily.”
The end goal, Perez-Cruet said, is to prepare medical students to practice in a world increasingly impacted by climate change and empower them to take mitigative and adaptive measures.
“Health-care sector engagement is imperative to climate change mitigation and adaptation,” he said. “We all took a pledge to do no harm at the very beginning of our training, and yet we contribute disproportionately to environmental degradation as a sector.”
Impact of health care on climate
The health-care industry is among the largest sources of greenhouse gas pollution. Accounting for 8.5% of domestic carbon emissions, the carbon footprint of the U.S. health-care industry alone would rank 13th among countries. Hospitals require more than six times as much electricity per square foot as an average home, and cooling hospitals equates to the emissions from 75 million cars each year.
These emissions raise a concerning paradox seldom discussed in hospital wards: the harmful health impacts of health care itself as an industry.
“I think you can get paralyzed by the scope of the problem,” Perez-Cruet said. “But advocacy is about putting your actions behind your words.”
As just one example of advocacy, the Medical Campus has taken aim at volatile gases used during operative procedures.
In 2016, Barnes-Jewish Hospital spent close to $1 million on volatile anesthetics. Much of this was spent on desflurane, the most expensive volatile agent, which has the advantage of quickly leaving the body after procedures. This is particularly advantageous in patients who are overweight or obese.
Desflurane, however, has approximately 2,540 times the carbon footprint of carbon dioxide. To make things worse, if administered at unnecessarily high flow rates, most of it escapes to the atmosphere without entering the patient.
When administered at high flow rates, one hour of desflurane use in a single patient can generate a carbon footprint comparable to driving more than 300 miles — a drive from St. Louis to Nashville. By comparison, the footprint of a similar agent, sevoflurane, equates to about eight miles.
“We need to be cognizant of the medical costs and benefits but also of the environmental costs and benefits,” said Ryan Guffey, MD, an anesthesiologist who helped spearhead the initiative. “The environmental costs of treatments aren’t on the drug label.”
A group — including Guffey, Helga Komen, MD, assistant professor of anesthesiology, and Ivan Kangrga, MD, PhD, professor and director of clinical anesthesiology — drafted guidelines for WashU Medicine anesthesia clinicians to use desflurane only in specific situations in which it would make a clinical difference.
They partnered with the Barnes-Jewish Hospital pharmacy to create a training module for anesthesia clinicians. The group also collaborated with the Anesthesia Control Tower, an innovative telemedicine team launched by the anesthesiology department, to develop a clinical decision support program. This program alerts clinicians if the flow rates of desflurane or other volatile agents are unnecessarily high.
The group expanded to include Perez-Cruet and third-year medical student Caellagh Catley and is working to analyze the longitudinal outcomes of these interventions. Use of desflurane has plummeted. By 2019, the usage was only one-quarter of its 2016 levels, amounting to a savings of $400,000 annually and a carbon footprint reduction of 60% — all with no effect on patient outcomes. Led by this anesthesiology department initiative, Barnes-Jewish Hospital has practically become a desflurane-free facility.
On the heels of its success with volatile anesthetics, the Department of Anesthesiology has begun taking steps to drive down its use of gases even further. The department is relying less on inhaled gases for delivering intraoperative anesthesia and instead using intravenous anesthetics, such as propofol.
Climate change & clinical practice
While climate change affects health care at the macro level, a warming planet already has begun to change providers’ day-to-day interactions with patients. Warmer temperatures can push the geographic boundaries of where certain diseases would be expected and bring more patients in with asthma and heat-related complaints.
A growing body of evidence has focused on the effects of climate change in facilitating the evolution of multidrug-resistant superbugs. Jason P. Burnham, MD, assistant professor of medicine, published a review in 2021 that has laid the groundwork for future research into these links.
The picture it paints of the future of antibiotic resistance can be as clear-cut as it is uncertain. Microplastics in waterways have been found to act as a collecting point for bacteria to share genes. Pollution, fertilizer use and warmer temperatures all can promote mutation formation as well, accelerating antibiotic resistance and unbalancing ecosystems’ ability to keep infectious diseases in check.
Burnham poses one scenario: A currently treatable bacteria species endemic to the Gulf of Mexico is routinely exposed to fertilizer from the Mississippi River and pollution from chemical companies along the Gulf while it collects on microplastics. Increasingly severe hurricane seasons fling these newly hardened germs farther inland, where shifting temperatures allow them to gain a foothold.
But, he points out, it isn’t always easy to determine precisely how ecological factors add up to clinical changes.
“Drought is surprisingly good for malaria because it kills off mosquitoes’ predators,” Burnham said. “So you can get more malaria when it’s dry, even though you would think there would be more mosquitoes when it’s wet because of more standing water.”
Looking at all of these factors operating together will be crucial for understanding and predicting antibiotic resistance and other mutations in the years ahead.
“Many fungi struggle to live at human body temperature, which is why most fungal infections occur in immunocompromised patients,” said infectious disease and critical care fellow Patrick B. Mazi, MD. “The fungi cannot overcome the less-than-ideal temperature and a normal immune system. But if they were to adapt to living at human body temperatures, it would be extremely problematic.
“If you look at the history of species-level extinction events, they are frequently caused by fungi. It’s typically not viruses, not bacteria, for the most part. As an example, amphibians are ectothermic and don’t have higher body temperatures to provide some protection against fungal pathogens. As a result, a single type of fungal infection, chytridiomycosis, has ripped through the environment resulting in the extinction of nearly 100 amphibian species.”
Mazi is working with other WashU Medicine researchers to reexamine our understanding of how fungal infections are distributed in the U.S.
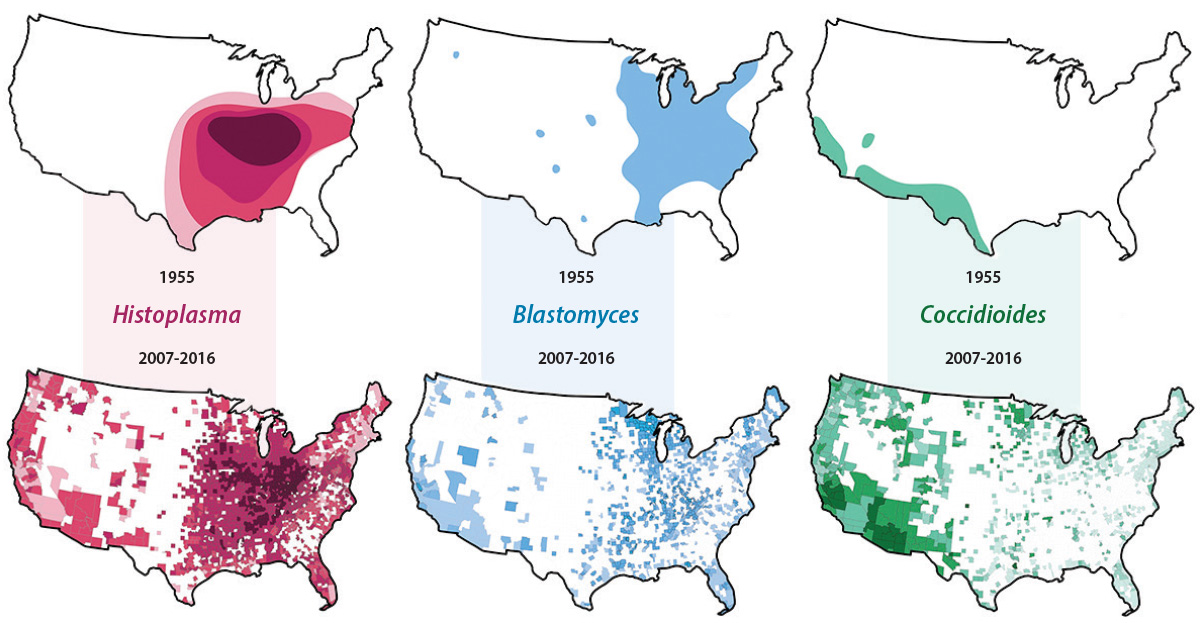
Their work takes aim at key assumptions doctors are trained to make about North America’s endemic fungal infections, called mycoses. For most medical board exams, trainees are expected to use geography to help guide their diagnosis. Histoplasma species, for example, are traditionally known to lurk in the Ohio River Valley, whereas Blastomycosis is associated with the northern Midwest, and Coccidiomycosis inhabits the arid Southwest.
These observations, however, relied on a study that was conducted more than 70 years ago.
The group’s database showed that the locations where fungal mycoses thrive, likely due to climate change, are much more widespread than their previously assumed distributions. Mazi has called into question whether the label of “endemic,” meaning pertaining to a geographical area, should be used at all. “I almost never bet against fungus when it comes to being able to adapt in an environment,” he said.
While many patients overcome such infections relatively unscathed with a recoverable form of pneumonia, a more accurate map reflecting the movement of mycoses could prove lifesaving for the growing number of Americans who are living with compromised immune systems. For such patients, a fungal infection may pose serious — sometimes fatal — risks.
“Every few weeks I get a call from a doctor in the northeast U.S. — a different doctor every time — about a case they can’t solve,” said senior author Andrej Spec, MD, an associate professor of medicine and a specialist in fungal infections. “They always start by saying, ‘We don’t have histo here, but it really kind of looks like histo.’ I say, ‘You guys call me all the time about this. You do have histo.’”
The team also created mycoses.org, which helps physicians quickly look up the incidence of endemic fungal infections in an area.
Climate change is redrawing the clinical map, and new tools — and vigilance — are required to make sense of these changes so that clinicians can optimize care for their patients.
From world-class work on fungi to eliminating harmful greenhouse gases to innovative medical education scholarship, WashU Medicine increasingly has been marshaling its resources as an academic powerhouse — pushing our understanding of how climate changes will affect human health and developing tools for mitigation.
Published in the Spring 2023 issue








 Share
Share Tweet
Tweet Email
Email