Their mother’s death when they were teenagers set identical twins Obi and Malachi Griffith on a shared path to find better cancer therapies. Today, the twins, both geneticists and computational biologists at the School of Medicine, are seeking precision treatments for the disease. The Griffith Lab, driven by the twins’ independent and complementary research interests, is a large team of biologists, bioinformaticians, computer scientists and software engineers.
One of the lab’s key developments is a free, open-source database that matches cancer mutations found in patients’ tumors with drugs targeting such genetic errors. The database, called CIViC, stands for Clinical Interpretations of Variants in Cancer. With CIViC, doctors treating unfamiliar forms of cancer can quickly comb the available medical research to find insights for their patients.
The Griffiths compare CIViC to the online encyclopedia Wikipedia, which similarly is maintained and updated by volunteers. Anyone can create an account and contribute information to the CIViC database. Experts in the field serve as CIViC editors, curating data that is incorporated into the system.

Maintaining up-to-date, comprehensive information about genetic mutations — and what those mutations may mean for patients — is a major bottleneck to improving cancer care.
“Often, doctors have some genetic information about a patient’s tumor, but it’s not clear what that might mean for treatment,” said Obi Griffith, PhD, an associate professor of medicine and of genetics. “Searching the scientific literature is time-consuming, and important data could be missed.
“The purpose of CIViC is to streamline and automate that process,” he added. “It’s a resource that can help clinicians determine the specific type of cancer a patient has, the prognosis and, in some cases, identify a drug that has the potential to help the patient.”
CIViC users span 163 countries. Many opt to receive automated CIViC updates so they can be incorporated into diagnostic or clinical workflows.
The National Cancer Institute of the National Institutes of Health (NIH) recently provided $3.7 million in new support for the database project.
It’s easy to wonder whether the existence of a tool like CIViC could have helped the twins’ mother 23 years ago.
Overcome by grief
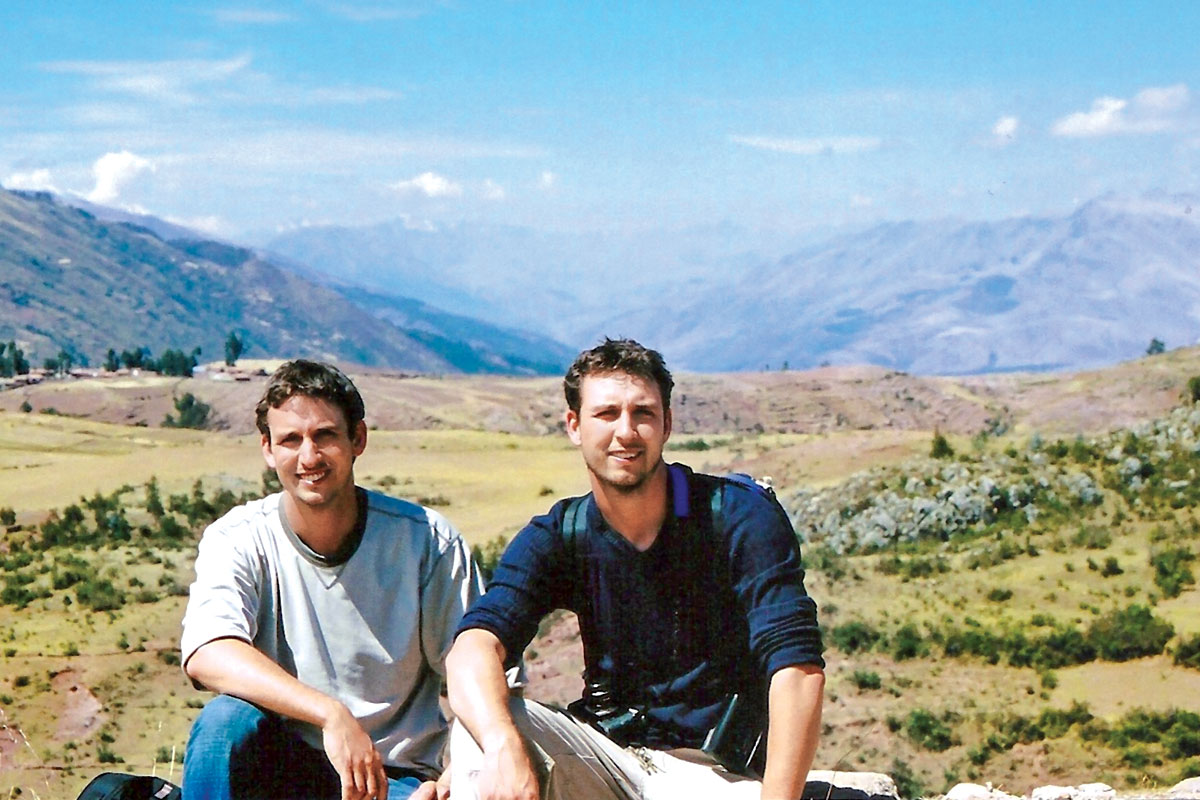
The Griffiths grew up on a tree farm in Manitoba, Canada, and spent free time helping their father run his landscaping business. Their childhood and early teenage years were lived outdoors, with lots of canoeing, hiking and fishing, and attending the occasional summer science camp.
Their world was shaken during their junior year of high school, when their mother was diagnosed with breast cancer. She was treated with the standard care available at the time. The treatment was not effective, and she died just weeks before their high school graduation.
“We were in a state of shock,” said Malachi Griffith, PhD, an assistant professor of medicine and of genetics. “I think our father felt like college would be a good distraction. It was sort of a heads-down, get-to-work approach to grieving, which has pros and cons.”
Obi added, “We did well that year academically, but it was miserable.”
“It’s hard to focus on complicated intellectual tasks, like getting a degree in biochemistry, when you’re really distracted by grief.” – Malachi Griffith, PhD
Relatively soon after her death, other family members were diagnosed with different forms of the disease. A cousin developed Burkitt lymphoma, a form of non-Hodgkin’s lymphoma. And a stepbrother was diagnosed with Ewing sarcoma, a bone cancer most commonly found in rapidly growing teenagers.
Cancer, although quickly fatal for the twins’ mom, was curable for their cousin and stepbrother. Why were the outcomes so different? This question would haunt them. As early undergraduates — before they had the education and skills for that question to crystallize in their minds — the brothers realized they needed a break.

“It’s hard to focus on complicated intellectual tasks, like getting a degree in biochemistry, when you’re really distracted by grief,” Malachi said. “We needed time to reset, so we took a gap year after our first year of college. As far as personal and emotional healing, the break was extremely important.”
Obi added, “A lot of adults around us questioned whether it was a good idea. But we didn’t share their concerns.”
With two high school friends, Obi and Malachi left the University of Winnipeg and drove west across Canada and north to the Yukon Territory, where they fished and hiked and canoed several hundred miles down the Teslin River. Over the next year, they made their way south down the Pacific Coast to Mexico, where they explored archeological sites and swam in the ocean.
“It was a great experience — playing chess in an orange camper van on some paradise beach in the middle-of-nowhere Mexico,” Malachi said. “But we were living on rice and beans and working odd jobs for gas money, so it didn’t take long to recognize that it was important to return to our studies. Still, for anyone dealing with traumatic loss — if you can swing it — I highly recommend that kind of reset.”
Embracing bioinformatics
The brothers returned to the University of Winnipeg and finished their biochemistry bachelor’s degrees with what seemed to be unfortunate timing. It was 2002, and the so-called “dot-com bubble” had burst, flooding the job market with skilled biotechnology workers all looking for employment.
The twins began to realize they would need more education and started discussing this “new thing” called bioinformatics. After an internet search for the term, Obi zeroed in on Vancouver.
“Steven Jones was doing bioinformatics work at the British Columbia (BC) Cancer Agency,” Obi said. “So I gave him a call. He listened to my background and offered me a job. He remains head of bioinformatics there. Even now, it’s hard to find people with a specific bioinformatics background. The field is basically looking for people who understand genetics and biology and aren’t afraid of computers.”
Malachi soon got a job at the BC Cancer Agency in a similar informal fashion. In the early 2000s, at the height of the Human Genome Project’s race to sequence the complete DNA of the human genome, the fields of genomics and bioinformatics were just taking off. The Griffiths consider themselves fortunate to be among the first people hired by the BC Cancer Agency as its bioinformatics research group was rapidly expanding.
Then, cancer struck again: Malachi’s supervisor was diagnosed with a brain tumor. He managed to survive against seemingly impossible odds.
“At some point not terribly long ago, all of these cancers — breast cancer, Ewing sarcoma, Burkitt lymphoma, brain tumors — all of them were a death sentence, and many still are,” Malachi said. “We’re making progress, but still, why can we stop some tumors but not others?”
Ultimately, the question would bring them to Washington University. The Griffiths had completed doctorates in medical genetics at the University of British Columbia, Vancouver, and conducted postdoctoral research in Vancouver and Berkeley, Calif. For the Griffiths’ next move, Washington University offered three crucial advantages: cutting-edge genomics with big data sets; top computer science and bioinformatics specialists; and an affiliated cancer hospital treating patients — opening the door for new discoveries to impact patient care.

A lifesaving clue
After joining the School of Medicine, the twins learned that a young, fellow cancer researcher, Lukas Wartman, MD, was battling a recurrence of the disease he now studies, acute lymphoblastic leukemia (ALL). In a race against time, this relapse prompted an ensemble team to harness all the tools and skills it had been building to save lives.
Wartman had been diagnosed with ALL while still a Washington University medical student. A first round of chemotherapy led to a five-year remission. He graduated in 2005 and undertook an internal medicine residency and hematology/oncology fellowships. A relapse in 2008 was treated with a bone marrow transplant from a matched donor, and that remission lasted until 2011, when he relapsed a second time.
A second relapse in adult ALL is usually incurable and quickly fatal. But Wartman joined a research protocol led by Timothy Ley, MD, the Lewis T. & Rosalind B. Apple Professor of Medicine, who was conducting genomic sequencing of patients with lymphoid cancers.
Whole-genome sequencing and the sequencing of the protein coding regions of Wartman’s cancer’s DNA did not reveal any routes to therapy. Sequencing of RNA — a close chemical relative of DNA — provided a clue: one protein, while normal in its sequence, was being produced by the tumor in far higher amounts than normal.
“At the time, I was trying to automate and streamline different kinds of genomic analyses, combining DNA and RNA sequencing data, along with many computational approaches for interpreting these data,” Malachi said. “We wanted to look at genes that were outliers inside this tumor. I remember sending an email summary of that case around to the leading investigators. I didn’t see any mutations, but there was one gene — FLT3 — that was extremely highly expressed. Tim Ley wrote back within a few minutes, saying that we should dig further — as this finding could be important.”
FLT3 had never been implicated in ALL but was widely known to drive kidney cancer and other tumor types. And there was a drug to treat it. Based on this analysis, Wartman began taking the drug sunitinib, a FLT3 inhibitor. Wartman, MD, now an assistant professor of medicine, has described the result as miraculous and lifesaving.
The result is precisely the kind of discovery that the Griffiths hope to make more common for cancer patients who have run out of options.
The early work that led to Wartman’s lifesaving treatment — in automating and streamlining genomic analysis — has expanded and grown into CIViC.
More recently, the Griffiths started working with their colleagues to design personalized cancer vaccines. Using genomic analysis and bioinformatics, they are predicting which misshapen proteins (characteristic of a specific patient’s tumor) will be most likely to trigger T cells to mount a powerful immune response.
“There are now seven clinical trials going on at Washington University looking at various personalized cancer vaccines, including for breast and brain cancers,” Obi said.
“Expanding the CIViC knowledge base and developing cancer vaccines are two very different approaches to personalized treatments for cancer,” he added, “but they both harness the genomics and bioinformatics tools that we’re working to build, in an effort to help more patients.”
Julia Evangelou Strait is a senior medical sciences writer in Medical Public Affairs.

Published in the Winter 2019-20 issue








 Share
Share Tweet
Tweet Email
Email