Pull on any loop of the Gordian knot that is finding treatments for pain and addiction, and the whole knot just tightens. Powerful painkillers come with a daunting risk of chemical dependency. The persistent sadness, worry and inability to find joy in life that can accompany chronic pain make substance use more appealing.
“Understanding pain and addiction is one of the most pressing needs in health care,” said Michael S. Avidan, MBBCh, the head of the Department of Anesthesiology and anesthesiologist-in-chief at Barnes-Jewish Hospital. “The way we treat pain has exacerbated the opioid epidemic, which is one of the biggest scourges in our society. We’re not going to solve this by waging a war on drugs. We’re going to address this by understanding the mechanisms of pain, why addiction occurs and by translating scientific insights into clinical practice.”
It’s in your genes
There’s a persistent myth that behavioral disorders are less grounded in biology than physical diseases such as diabetes, and therefore less treatable. Psychiatrist Laura Bierut, MD, has helped prove that idea false through her work on the role of genetic factors in smoking, alcoholism and other substance-use disorders. Among other things, she has identified genes that influence a person’s risk of becoming a heavy smoker and of developing lung cancer, and showed that providing smokers with personalized risk information based on their genetics helps them kick the habit.
Pain and pleasure
It’s hard to be happy when you’re always hurting. That’s one reason opioids can be so addictive — they dampen both physical and emotional pain, leaving people temporarily pain-free and euphoric. Neuroscientists Meaghan C. Creed, PhD, and Jose A. Moron-Concepcion, PhD, have identified circuitry in the brain that links pain to negative emotions such as sadness, anxiety and an inability to feel joy. The finding suggests that modulating the circuitry could treat both emotional and physical suffering, an approach that could reduce the addictive potential of opioids and improve quality of life for people with chronic pain, even when it’s not possible to completely eliminate pain itself.
“By targeting the emotional aspects of pain, we hope to make pain less debilitating so that patients won’t crave the emotional high they get from opioids.”
— Jose A. Moron-Concepcion, PhD
Nonaddictive pain relief

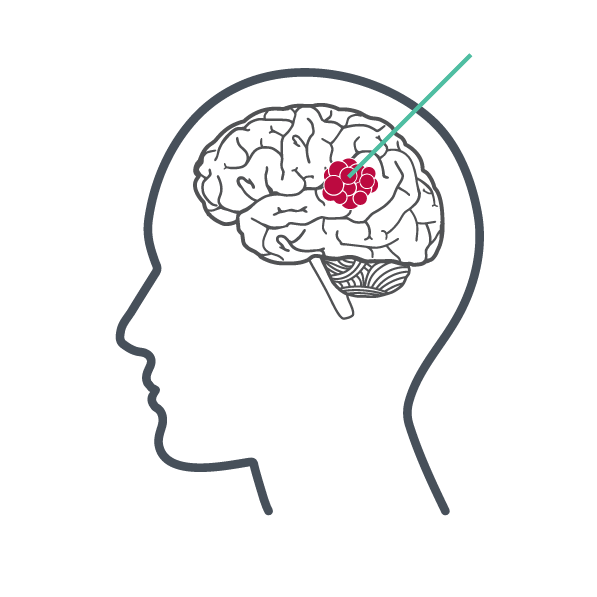
The devastating and deadly ongoing opioid epidemic highlights the difficulty of balancing the need for pain relief against the dangers of addiction. Pain scientist Robert W. Gereau IV, PhD, studies how pain signals are transmitted from the body to the brain with the aim of finding new ways to alleviate pain. He has created a tiny, flexible LED device that can be implanted in body parts that experience persistent pain to interrupt the transmission of pain signals. In other work, pharmacologist Susruta Majumdar, PhD, is working on improving the safety profile of fentanyl, a powerful opioid pain reliever and the leading cause of opioid overdose deaths. He has created an altered fentanyl molecule that he expects will be less lethal and addictive but still able to alleviate pain.
Navigate the neurosciences
Continue exploring the extensive scope of neuroscience research conducted at WashU Medicine.
Published in the Winter 2023-24 issue









 Share
Share Tweet
Tweet Email
Email